We don’t always think about how race and racism affect health care. Yet, according to the Ontario Human Rights Commission (OHRC), racial inequality and inequity in health care are often indirect, subtle and systemic. This poses a challenge for us all, as inequitable societies are shown to have higher rates of crime, obesity, incidences of mental illness, and infant mortality rates.[1] Understanding the health disparities that racialized and Indigenous people face, can help in the struggle to achieve equitable care for all Canadians.
Across Canada, one of the biggest gaps in healthcare is the lack of available data around race. According to the Globe and Mail, Canada’s data void around race and ethnicity is stark when compared with other countries, who use this data to inform healthcare policy and better target problems, by showing whether certain groups are more prone to specific diseases. If we were to gather more data around race and the lived experiences of racialized communities here in Canada, researchers widely believe that we would reveal some very uncomfortable truths.[2]
- What We Know About Health Inequity and Race
- How Covid-19 Highlighted Health Inequality
- How Wealth Affects Health
- Racism in Health Care
- Bottom Line
What We Know About Health Inequity and Race
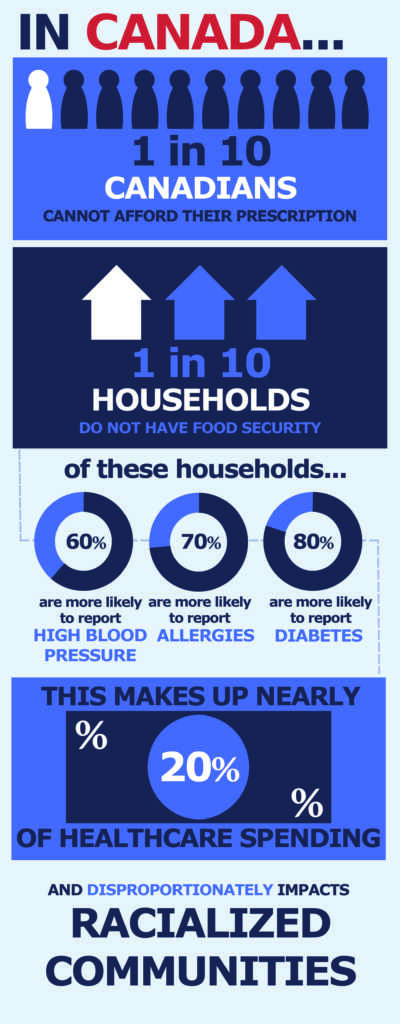
1 in 10 Canadians cannot afford to fill their medical prescriptions and almost 4 million households experience food insecurity. These same households are 80% more likely to report having diabetes, 60% more likely to report high blood pressure, and 70% more likely to report food allergies. Such disparities in the health system makeup almost 20% of healthcare spending and disproportionately impact racialized communities.[3]
We know this, because 1 in 5 racialized families live in poverty in Canada, as opposed to 1 in 20 non-racialized families. Additionally, the wage gap between Black individuals and the rest of the population in Canada has grown over the last twenty years. For example, Black men and women living in Alberta’s biggest cities make significantly less money than their non-Black counterparts. Black women and men in both Calgary and Edmonton are between 1.5 to 2 times more likely to be unemployed than the rest of the population. This statistic persists nationally, even within groups that have achieved the same level of education[4].
How Covid-19 Highlighted Health Inequality
Just last week, the city of Toronto released a sobering new data set that highlights what has been speculated for the past few months with regards to the Covid-19 pandemic: racialized communities and those from low-income households have been disproportionately infected. Those belonging to racialized groups in Toronto make up over 80 percent of Covid-19 cases within the city[5]. What the data shows is that those individuals and communities which face systemic barriers are at a much higher risk of contracting Covid-19. These barriers include poverty, racism, unequal access to services, and sometimes all of the above.
Those belonging to racialized groups in Toronto make up over 80 percent of COVID-19 cases within the city
How Wealth Affects Health
Why is all of this important? Because the past and present context of wealth inequities serve as perfect examples of how privilege works in institutions such as health care.
Canada’s middle class has shrunk since the 1990s, as income has stagnated and poverty levels have grown. What we know about this, is that where kids land on the economic ladder is based more on their parents’ status rather than their own hard work and talents. Despite this, the idea that people get opportunities and succeed based primarily on their talent and effort persists. In other words – whatever one ends up with must be what that individual worked hard for, earned and deserved. It asserts that race, gender or discriminatory factors do not play a role in determining success. However what the data tells us is that this is simply not the case, socioeconomic factors and feelings of safety and wellbeing play a significant role in our overall health[6].
For example, those who endure instances of racial profiling or targeted harassment —be they subtle or violent—do not escape unaffected. They often suffer from post-traumatic stress disorder, and this trauma, in turn, affects their friends, families and immediate communities, who are then exposed to their own vulnerability as a result. What’s more, researchers have noted that external stressors such as racism can have a permanent impact on physical health in addition to mental health – a key component of stress-related disease[7].
Those who endure…racial profiling or targeted harassment…often suffer from post-traumatic stress disorder, and this trauma, in turn, affects their friends, families and immediate communities
Racism in Health Care
For Canada’s Indigenous people, health care has been a major site of harm. A now-famous example is that of Brian Sinclair, an Anishinaabe man who went to Winnipeg’s Health Sciences Centre for a treatable bladder infection. Mr. Sinclair actively sought out health care services, yet was continually told to wait. After waiting thirty-four hours in the emergency waiting room, without being seen by a physician, he was discovered dead. This denial of care for Mr. Sinclair has been attributed to anti-Indigenous racism and stereotyping, whereby he was seen as homeless and drunk, rather than as a patient in need of and deserving of care[8].
The history of interactions between colonial peoples and Indigenous peoples is a key part of the current and past health history of Indigenous people in what is now Canada. Current health issues are irrevocably tied to historical patterns of exploitation, trauma and disenfranchisement with respect to resources and access to health care[9]. These patterns continue to persist through structures of racism that are so deeply interwoven into our societal fabric, that they influence every aspect of our lives.
Bottom Line
Reducing these inequities requires a societal commitment to reducing racial inequities in our health care systems in a systematic and sustained way. I hope conversations such as this, serve as an invitation to engage in efforts in which we can all use our advantages to share power, create space, call out unjust or inequitable practices and strive towards equity.
Article By:
Zahra Ismail, BA, MA, M.Ed
Zahra Ismail is an educator and practitioner whose work explores transformative approaches to peacebuilding, human rights, and social justice in education in diverse contexts.
Edited and Reviewed By The Health Aisle Team
References:
1. Even it Up: Time to End Extreme Inequality. Retrieved from https://www-cdn.oxfam.org/s3fs-public/file_attachments/cr-even-it-up-extreme-inequality-291014-en.pdf
2. Grant, T., & Balkissoon, D. (2019, February 11). How Canada’s racial data gaps can be hazardous to your health. Retrieved from https://www.theglobeandmail.com/canada/article-how-canadas-racial-data-gaps-can-be-hazardous-to-your-health-and/
3. Neidhart, L. (2020, July 29). Just the Facts. Retrieved from https://cwp-csp.ca/poverty/just-the-facts/
4. Racial inequality in Alberta, by the numbers | CBC News. (2020, June 19). Retrieved from https://www.cbc.ca/news/canada/calgary/racial-inequality-alberty-numbers-gaps-1.5614929
5. Black people and other people of colour make up 83% of reported COVID-19 cases in Toronto | CBC News. (2020, August 02). Retrieved from https://www.cbc.ca/news/canada/toronto/toronto-covid-19-data-1.5669091
6. Institute of Medicine (US) Committee on Assessing Interactions Among Social, Behavioral, and Genetic Factors in Health; Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington (DC): National Academies Press (US); 2006. 2, The Impact of Social and Cultural Environment on Health. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19924/
7. Physiological responses to racism and discrimination: an assessment of the evidence. American journal of public health, 93(2), 243–248. https://doi.org/10.2105/ajph.93.2.243
8. Nestel, Sheryl. Color Coded Health Care. http://www.wellesleyinstitute.com/wp-content/uploads/2012/02/Colour-Coded-Health-Care-Sheryl-Nestel.pdf
9. June 2, 2. ·, & Tags: Alison Reiheld, A. P. (2018, January 02). Canada’s Biggest Health Problem: Indigenous Health. Retrieved from https://impactethics.ca/2017/06/02/canadas-biggest-health-problem-indigenous-health/


Leave a Comment