Taking a comprehensive, whole-person approach with the guidance of a Naturopathic Doctor may better help in understanding your migraines and bring long-term relief. Gathering the right information and exploring root causes are big steps towards understanding your migraines. Here are some frameworks, what to track and some things to think about:
- Why Should I Bother Understanding My Migraines?
- How Common are Migraines?
- What are Migraines?
- What Migraine Symptoms Should I Track?
- What Other Symptoms Should I Track for my Naturopathic Doctor?
- What Other Tests Can Be Done to Assess What is Triggering my Migraines?
- Bottom Line
Why Should I Bother Understanding My Migraines?
Understanding your migraines will help you discover why they happen, determine your individual triggers, and how to better manage (even prevent) them before they start. This can also help you make the right changes for your body and get faster and better pain relief.

How Common are Migraines?
Studies show that over 1 in 4 people across North America have experienced a migraine at one point in their lives.
Many people opt for a natural solution first to treat their migraines; however, it may be necessary to take a multi-dimensional approach because a medication-free migraine cure is not always possible. (Read about Roopa’s story here). Everyone’s approach will be unique.
What are Migraines?
Through most of the 20th century, migraines were thought to be vascular in nature, involving the blood vessel; therefore, treatment with ergotamine was common. Then research revealed that there is a neurological component of the pain that came before the blood vessel spasms. Migraines are now considered a neurovascular condition, involving the trigeminal nerve and the blood vessels, triggering pain receptors. They are now more successfully treated pharmaceutically with triptans.
The phases of the migraine include:
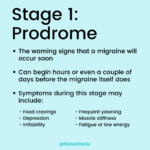
- Prodrome phase, which may include symptoms such as nausea and sensitivity to light
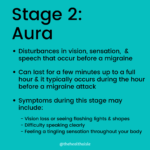
- Aura phase, which may include nerve-like sensations in the arms
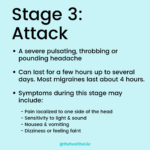
- The migraine attack itself, and then the
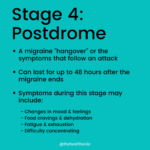
- Post-drome phase, often involving a long period of deep sleep.
What Migraine Symptoms Should I Track?
Keeping a detailed headache diary or journal can be a useful tool to determine what happens alongside a headache. This may include period tracking (hormonal changes), digestive symptoms or other any other symptoms you notice such as leg cramps, diarrhea, food poisoning, constipation, heavy bleeding, irritability (as some examples).
This information is helpful for yourself and various health care providers in understanding your migraines.
Migraine signs and symptoms to track:
- Are you sensitive to light or sound?
- Do you get any warning signs before the migraine?
- Do you feel nauseated or vomit with migraines?
- Where on your head to you feel the headache (which side, point to it, track it if it changes)
- Timing – is it around your period? Before, during or after?
- How long do the migraines last for?
- Do you take any medications and do they HELP your migraine?
- When in the course of the migraine do you take these medications and at what dosage?
- How long does the medication help for?
- Do you have any associated symptoms that happen with your migraines?
- Do you need to sleep for a long period of time after your migraine?
- Stress factors or triggers in life that you’ve noticed?

What Other Symptoms Should I Track for my Naturopathic Doctor?
To fully arrive at an understanding of your body’s triggers and symptoms, a naturopathic doctor completes a Review of Systems. This is asking you about every system in your body in addition to the questions about the migraine themselves.
Here are some others conditions and things to look at that might help in understanding your migraines and what might be the cause or triggers:
- Skin rashes, eczema or acne
- Allergies
- seasonal/environmental allergies
- Food allergies and sensitivities to gluten and/or dairy
- Mold exposure/mycotoxin levels
- Heavy metal exposure
- IBS or IBD, Constipation or Diarrhea?
- Depression
- Body Pain / Chronic Fatigue
- Iron Deficiency signs
- Magnesium Deficiency signs
- Periods: are they regular or irregular? PMS
- Blood clots?
- Where is the headache? Eyes or back of the head?
- Nausea?
- Is it worse after drinking alcohol or smoking?
- Insomnia: What time are you waking up if waking up in the middle of the night?
- TCM Clock explanation
What Other Tests Can Be Done to Assess What is Triggering my Migraines?
A naturopathic doctor may also perform a standard physical examination or review reports if you had them done with your family doctor or specialist including a neurological exam.
Individualized tests may be done depending on access, individual signs and symptoms and budgetary considerations.
Laboratory testing is not always necessary to get a result for treatment, but it is good practice to consider especially if you reach a plateau in your treatment improvements.
Here are some guiding questions we ask to determine whether a test is necessary or not:
- Does it make sense to test based on the symptoms the person has?
- What is the specificity and sensitivity of the testing method itself?
- Do the benefits of this test outweigh the costs (financial and of the experience)?
- Is this test a reasonable next course of action?
- And if we did this test, would it change our next step in terms of treatment?
Here are some functional and environmental medicine tests that may be considered to better guide the treatment of someone with migraines:
- IgG Food sensitivity testing vs. elimination diet. As an example, diet restriction to help migraine (based on IgG antibodies) may be an effective strategy in reducing the frequency of migraine attacks[1]
- Mold & Mycotoxin testing
- Heavy metal testing
- Hormonal testing (if related to periods)
- Nutrient deficiencies: B2, B6, B12, Mg, Fe
- Zinc Tally
- Genetic and Genomic Testing. Note that general tests you can buy for yourself may not be as helpful in testing specific alleles as those done with the guidance of an environmental genomicists
When we have a good idea of the frequency and quality of the migraines, underlying cause of the migraines, key triggers, environmental exposures, nutrient deficiencies, we can treat accordingly.

Treat the Whole Person
Naturopathic Doctors prescribe recommendations that complement your pharmaceutical prescriptions, consider interactions between natural health products and medications.
When developing an individualized treatment for migraines, the overall the approach often looks something like this:
- Start with removing triggers and reducing inflammation. Often this includes identifying and addressing food sensitivities with a goal of 80/20 or 90% for some key triggers. We may also look at environmental exposures at home or in the workplace, such as mold.
- At the same time, we want to balance the imbalanced. This often involves optimizing your normal detox and elimination pathways, which helps balance your hormones. Three general food options I may recommend are:
- Indole-3-carbinol (I3C) sources such as broccoli, brussels sprouts, cabbage, collards, cauliflower, kale, mustard greens, turnips, and rutabagas (raw or lightly cooked to minimize goitrogenic impact if there is a risk of hypothyroidism)
- Fibre-rich foods
- Phytoestrogen-rich foods – depending on interactions with medications, these can be also good sources of fibre
- Nutrient deficiencies are also important to consider. Treatment options here include dietary support, supplements, as well as IV nutrient therapy. Some key nutrients to consider here are Magnesium and Vitamin B2, in addition to adequate hydration.
- Acupuncture is another modality that can be very useful when it comes to weaning off medications, especially acute migraines that can occur as you reduce your dosages. Acupuncture balances Qi and Blood – which is foundational to health and wellness in Traditional Chinese Medicine
- Herbal medicine has been used extensively for migraine support, as herbs can provide an anti-inflammatory effect and reduce spasms.
Bottom Line
Although migraines may feel impossible to treat, they don’t have to be. Understanding your migraines by identifying triggers and tracking the right the information that will better help identify root causes and discover the best treatment plan. A Naturopathic Doctor may be a good resource in helping you better understand your migraines and with with other health care professionals to find the best path forward.
Author(s):
Dr. Julie Hwang, ND
Owner & Founder of Aurum Medicine & Wellness Clinic located in Toronto, Canada. Integrating western diagnostics with traditional Chinese medicine approaches, her practice is focused on headaches, seizure disorders and eczema.
Edited and Reviewed By The Health Aisle Team
References
1. Alpay, K., Ertas, M., Kocasoy Orhan, E., Kanca Ustay, D., Lieners, C. and B. Baykan. Diet Restriction in Migraine, Based on IgG Against Foods: A Clinical Double-Blind, Randomised, Cross-Over Trial. Cephalalgia. 2010 Jul;30(7):829-37. doi: 10.1177/0333102410361404. Epub 2010 Mar 10. https://pubmed.ncbi.nlm.nih.gov/20647174/
2. Lipton, RB., Göbel, H., Einhäupl, KM, Wilks, K. and A Mauskop. Petasites Hybridus Root (Butterbur) Is an Effective Preventive Treatment for Migraine. Neurology. 2004 Dec 28;63(12):2240-4. doi: 10.1212/01.wnl.0000147290.68260.11. https://pubmed.ncbi.nlm.nih.gov/15623680/
3. Saranitzky, E., White, C.M.., Baker, E.L., Baker, W.L. and C.I. Coleman., Feverfew for Migraine Prophylaxis: A Systematic Review. J Diet Suppl. 2009;6(2):91-103. doi: 10.1080/19390210902861809. https://pubmed.ncbi.nlm.nih.gov/22435410/
4. Pareek, A., Suthar, M., Rathore, G. S. and Vijay Bansal. Feverfew (Tanacetum parthenium L.): A systematic review. Pharmacogn Rev. 2011 Jan-Jun; 5(9): 103–110. doi: 10.4103/0973-7847.79105. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3210009/
5. Goadsby, P., Holland, Philip R., Martins-Oliveira, M., Hoffmann, J., Schankin, C. and S. Akerman. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017 Apr; 97(2): 553–622. Published online 2017 Feb 8. doi: 10.1152/physrev.00034.2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539409/
6. Use of CAM in Patients with Migraine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353077/
7. Buse, Dawn C., Greisman, Jacob D., Baigi, Khosrow and Richard B. Lipton. Migraine Progression: A Systematic Review. Headache. 2019 Mar;59(3):306-338. doi: 10.1111/head.13459. Epub 2018 Dec 27. https://pubmed.ncbi.nlm.nih.gov/30589090/
8. Puledda, F., Mesina, R. and P. J. Goadsby. An update on migraine: current understanding and future directions. J Neurol. 2017; 264(9): 2031–2039. Published online 2017 Mar 20. doi: 10.1007/s00415-017-8434-y. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5587613/
9. Weatherall, M. The diagnosis and treatment of chronic migraine. Ther Adv Chronic Dis. 2015 May; 6(3): 115–123.doi: 10.1177/2040622315579627. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4416971/
10. Primary Headache Disorders: Focus on Migraine. Rev Pain. 2011 Dec; 5(4): 2–11. doi: 10.1177/204946371100500402. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590049/
11. Ong, Jonathan Jia Yuan and Milena De Felice. Migraine Treatment: Current Acute Medications and Their Potential Mechanisms of Action. Neurotherapeutics. 2018 Apr; 15(2): 274–290.
12. Published online 2017 Dec 12. doi: 10.1007/s13311-017-0592-1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5935632
13. Fenstermacher N, Levin M, Ward T. Pharmacological prevention of migraine. BMJ 2011; 342: d583. https://www.ncbi.nlm.nih.gov/pubmed/21335409.
14. Gilmore B, Michael M. Treatment of acute migraine headache. Am Fam Physician 2011; 83(3): 271-280. https://www.ncbi.nlm.nih.gov/pubmed/21302868
15. Harris P, Loveman E, Clegg A, Easton S, Berry N. Systematic review of cognitive behavioural therapy for the management of headaches and migraines in adults. Br J Pain 2015; 9(4): 213-224. https://www.ncbi.nlm.nih.gov/pubmed/26526604
16. International Headache Society (IHS). The International Classification of Headache Disorders 3rd edition (Beta version). 2016.
17. Kindelan-Calvo P, Gil-Martinez A, Paris-Alemany A, Pardo-Montero J, Munoz-Garcia D, Angulo-Diaz-Parreno S et al. Effectiveness of therapeutic patient education for adults with migraine. A systematic review and meta-analysis of randomized controlled trials. Pain Med 2014; 15(9): 1619-1636.
18. Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: A systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci 2017; 372: 307-315. https://www.ncbi.nlm.nih.gov/pubmed/28017235
19. Herbal Therapy in Migraine. https://pubmed.ncbi.nlm.nih.gov/24867850/
20. Foods and Supplements in the Management of Migraine Headaches https://pubmed.ncbi.nlm.nih.gov/19454881/
21. Non-Pharmacological approaches to Migraine Headaches. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5935652/
22. Complementary and Alternative Medicine Use among Adults with Migraines/Severe Headaches https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3627391/
23. Levin, Morris. Herbal Treatment of Headache. Headache. 2012 Oct;52 Suppl 2:76-80. doi: 10.1111/j.1526-4610.2012.02234.x.https://pubmed.ncbi.nlm.nih.gov/23030536/
24. Effect of Yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014 Jul-Dec; 7(2): 126–132. doi:10.4103/0973-6131.133891. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4097897/
25. Molseberger, Albrecht. The role of Acupuncture in the Treatment of Migraine. CMAJ. 2012 Mar 6; 184(4): 391–392. doi: 10.1503/cmaj.112032. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291665/
26. Shaik, Munvar Miya and Siew Hua Gan. Vitamin Supplementation as Possible Prophylactic Treatment against Migraine with Aura and Menstrual Migraine. Biomed Res Int. 2015; 2015: 469529. Published online 2015 Feb 28. doi: 10.1155/2015/469529 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4359851/


Leave a Comment